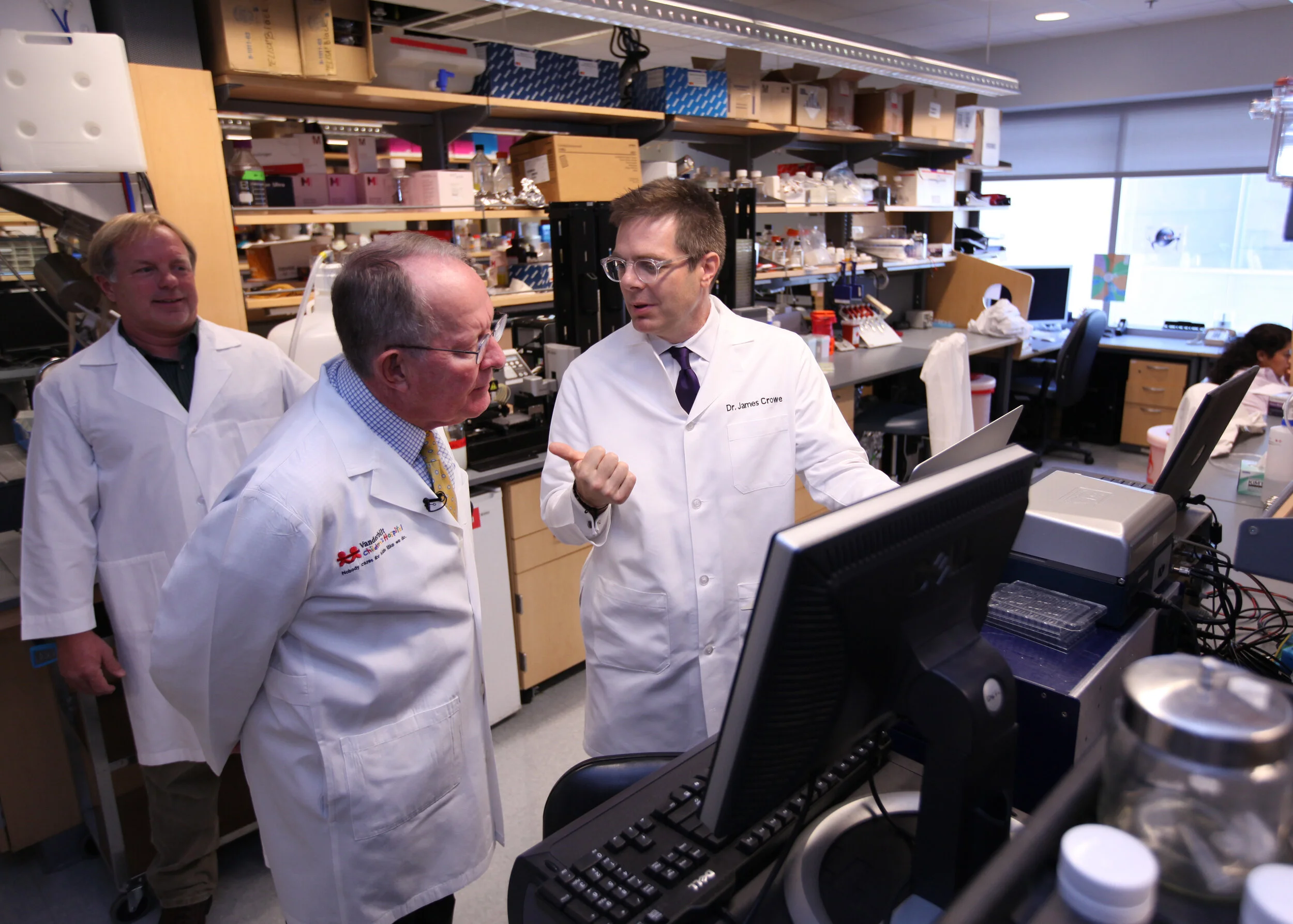
AWARDEE: James E. Crowe, Jr.
FEDERAL FUNDING AGENCIES: Department of Defense, National Institutes of Health
The Human Immunome: Small Moves Become a Movement
James E. Crowe, Jr.
“We’re basic scientists. We did not set out initially just to make drugs. That’s not what it was about when we started. I’ve just always been interested in how the human immune system even recognizes a virus,” says James E. Crowe, Jr., a well-known infectious disease expert who directs the Vanderbilt Vaccine Center in Nashville, Tennessee. “Now we can study how the body works and have curiosity about that, but also have drugs in the pipeline. It’s the unexpected benefit we get by delving deeply into the human immune system.” Crowe is one of the recipients of the 2020 Golden Goose COVID-19 Recognition for his decades-long pursuit of a better understanding of the human immune system, which is now paying dividends in the fight against COVID-19.
Investigating the Immune System
A pediatrician by training, Crowe spent part of his time in medical school caring for children in developing countries, where he saw the difference that access to health care could make. Vaccines held a particular interest. He was inspired by the advent of the life-changing polio vaccine, so much that he decided to join the lab of the late Robert Chanock, who led vaccine research at the NIH campus in Bethesda, Maryland. “Because of this deep immersion,” he says, “I became interested in research and its potential to save the world from the consequences of many diseases.” In 1995, Crowe joined the Vanderbilt faculty, where he soon won an award for young investigators from the American Society for Microbiology (ASM). At the same ASM meeting was innovator Craig Venter, famous for his role in the Human Genome Project. Sitting in the audience, listening to Venter’s speech, Crowe began thinking about small moves in science that can lead to a movement. If Venter could do it with the genome, why couldn’t Crowe do it with the immune system?
Well, for one thing: The genes that encode antibodies, proteins that function in the body as soldiers against disease, are more complicated. “Antibodies are formed by a combination of genes. You can make over ten thousand combinations, almost to the scale of the genome, but the three genes used are not stitched end to end,” Crowe explains. The spaces between them, where the antibody genes are joined, are filled with random DNA sequences that lead to many times more combinations. Even more challenging? The antibody genes can mutate. Factoring in those mutations, the scale of trying to characterize the human immunome, the “parts list” of the human immune system, is immense—billions of times larger than the human genome.
The focus on antibodies appealed to Crowe’s sense of wonder at the complex forms and patterns to be found in a biodiverse world. “My fascination with the pattern in nature touches back to my childhood,” Crowe says. “I was a collector of rocks and seashells and stamps, and the idea was to get one of everything. The idea of sequencing every possible antibody gene of the billions possible spoke to me.”
At the time Crowe was beginning to launch the idea, another epidemic was tearing through the globe: AIDS. HIV, the virus that causes AIDS, was garnering significant scientific interest. Crowe received a grant from the National Institutes of Health (NIH) to study B cells, the type of immune cell that makes antibodies, and he began to sequence antibodies in patients who tested positive or negative for HIV. Since then, the field has advanced in areas such as genome sequencing, synthetic biology, and data analysis, and this advancement has enabled the groundbreaking work that Crowe and his colleagues are now doing to understand the human immune system. Despite the potential, “sometimes big science can get criticized for scope relative to return on investment,” says Crowe’s colleague Jennifer Pietenpol, who oversees research at the Vanderbilt University Medical Center. It was a perception that Crowe and his team had to consider as they ramped up their antibody work over the years. However, as Pietenpol shares, “the techniques developed and learnings from big projects typically benefit the entire discovery continuum.”
The Human Genome Project, for example, took 13 years and cost around $3 billion, and it raised similar questions. Today, next-generation DNA sequencers can do the same job in a day for less than $1,000. Motivated by such advances, in 2016 a public-private partnership called The Human Vaccines Project launched the Human Immunome Program, with Crowe as its scientific director. The decade-long, multi-million-dollar effort brings together the expertise of many different disciplines and partners—a clear example of “team science.” A stronger understanding of the immunome could offer the potential to tailor human immune response and better ward off illness.
Advances in immunology have also led to a focus on monoclonal antibodies, lab-produced proteins that can bind to substances in the body that cause disease. Crowe’s lab has been able to generate such antibodies to target viruses that include dengue, Ebola, HIV, influenza, norovirus, respiratory syncytial virus (RSV), rotavirus, Zika virus and others. Antibodies the lab made for Marburg virus and chikungunya virus are now being explored in clinical trials. As with genome sequencing, the isolation and production of such antibodies is becoming easier and cheaper for scientists.
A Serendipitous Delivery
Crowe knew his lab’s approach to antibodies could help when the first U.S. cases of COVID-19 emerged in Seattle—but before his lab could engage, he needed to get blood samples from the patients to his teammates. “We had to get a blood sample from the first U.S. case from Seattle to Nashville on a Saturday night,” Crowe recalls. What followed was a series of calls—and, like many Golden Goose stories, a little serendipity.
“I called my CEO and asked him to call the CEO of FedEx, because I figured they knew each other,” he says, noting that FedEx is also based in Tennessee. “They got it done! Someone in a Lincoln town car drove the sample to my home on Sunday morning, I walked it into work, and we were up and running.”
Crowe and his wife in Italy
Problem solving is a necessity, and not only in collecting viable samples. In Crowe’s case, this work often means devising new strategies on short notice. Case in point: He and his wife departed for a long-planned three-month sabbatical to Italy in February–just before the novel coronavirus swept that country. After 25 fast-paced years at Vanderbilt, Crowe had been excited to have time and space to do some strategic thinking about high impact work he wanted to do over the next decade. So he made preparations to manage his lab from afar. These plans quickly changed as COVID-19 spread and Italy became the next major hot spot; Crowe and his wife made it onto one of the last available flights home.
By then, he and his team had worked out the techniques they wanted to use to do the coronavirus antibody work. Fortuitously, the best blood samples arrived the day he got back to the lab. “You have to let the immune response mature over time to get the best antibodies,” he says. “We tracked down some people who had been infected in Wuhan in December and got their samples in March.”
Just how does a scientist track down blood samples in situations like this? One has to be part news junkie, part detective. Crowe and his colleagues would scan the headlines for cases, distribute flyers, and get in touch with research and public health contacts in other cities who could share publicly available information and spread the news of the lab’s efforts. Often, the patients who learned of the project were eager to help. One patient even came twice when called for a blood draw—the second time on the way to the airport at the crack of dawn.
Accelerated Work
As the team collected samples, they were also conducting the science at a vastly accelerated pace. Though Crowe’s work on the Human Immunome Program was the basis for the work his lab is doing to help solve COVID-19, it wasn’t a straight line from one to the other. Crowe also credits work funded by the Defense Advanced Research Projects Agency (DARPA) at the Department of Defense for enabling the lab to respond so quickly and efficiently to the pandemic.
Running in the Alps
In late 2017, the team received a grant from DARPA to take on a challenge: find a way to produce antibodies for any virus within 60 days of collecting a blood sample from a survivor. DARPA focuses on cutting-edge defense-related research and is often know for outside-the-box thinking; in this case, the aim was to protect American troops if they were to confront a deadly virus in the field. “We thought it sounded crazy—this type of work usually takes years—but that’s what DARPA does. It funds the crazy,” Crowe says.
The team decided to attempt the rapid production of Zika virus antibodies after a flare-up of the mosquito-borne disease that caused birth defects in several countries. “We took a sample, started the clock, and made Zika antibodies and fully tested them in 78 days. We had a lot of semi-disastrous stuff happen like instruments breaking, so we had already learned how to make mistakes, face unexpected accidents, and move on.” The team had begun planning a second simulation of an avian influenza outbreak for 2020 but pivoted in January to handling COVID-19 as it became clear how serious the new virus had become. “With COVID-19, we jumped right in. We worked at a scale that was unprecedented because we knew how to do this already. … Staying stuck or quitting is not acceptable. You have to move forward—like in improv comedy. It was bootstrapping with very few assets to start with, and this type of work is very exciting if the team works together well. Each person has to enjoy the freedom of curiosity and extemporaneous ideas, while working up to 20 hours a day with urgent goals and timelines.”
With the blood samples they received from the Wuhan patients, Crowe and his team made thousands of monoclonal antibodies. After selecting the most promising ones and rapidly testing them against the virus in animal models, they sent the leading candidates for antibody tests and treatments to pharmaceutical companies. The first antibody sequences, which went to Astra Zeneca, have now led to potential treatments being tested in five different Phase 3 clinical trials. Some of the antibodies also are being readied for clinical trials by the U.S. government’s Joint Program Executive Office for Chemical, Biological, Radiological and Nuclear Defense (JPEO-CBRND). “In the context of this pandemic,” says Pietenpol, “the Crowe team’s pursuit of large-scale antibody science is returning milestone advances for the prevention and treatment of COVID-19.”
Crowe points out the importance of having multiple federal agencies with different missions and approaches, like NIH, DARPA, and the Biomedical Advanced Research and Development Authority (BARDA) supporting scientific research. “[COVID-19] is the best case I’ve ever seen where the agencies were all working together” toward the same goal, he says. He sees it as a testament to what federal R&D can accomplish to help solve pressing public health problems—now and in the future.
By Meredith Asbury