AWARDEES: Tibor Juhasz, Ron Kurtz, Detao Du, Gérard Mourou, and Donna Strickland
FEDERAL FUNDING AGENCIES: Department of Energy, National Science Foundation
Nearly 30 years ago, a graduate student at the University of Michigan's Center for Ultrafast Optical Science (CUOS) experienced an accidental laser injury to his eye. Fortunately, his vision was not severely affected; however, the evident exact and perfectly circular damage produced by the laser led to an exciting collaboration. Eight years later, that collaboration developed a bladeless approach to corrective eye surgery. The new procedure, also known as bladeless LASIK, uses a femtosecond laser rather than a precision scalpel to cut into the human cornea before it is reshaped to improve the patient’s vision.
Since 2002, 24 million people have benefited from the bladeless LASIK approach, which limits complications and broadens the pool of eligible patients. It is now considered the standard in the field.
It Only Takes a “Pulse”
In 1953, a 2012 Golden Goose Awardee, Charles H. Townes, built the first microwave amplification by stimulated emission of radiation, maser for short, and thereby introduced the world to the principle of laser technology. While he encountered many doubters who saw little value in the technology, the scientific community began to explore and advance ways to create more intense pulses.
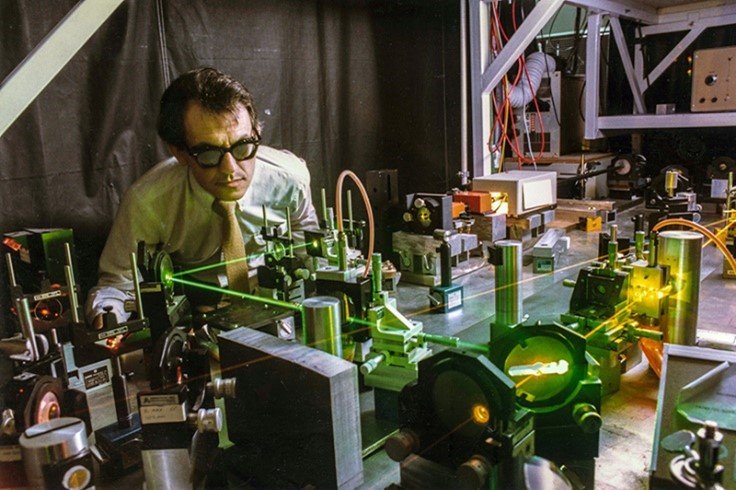
Gérard Mourou in the LLE lab at the University of Rochester
The U.S. Department of Energy defined the field of ultrafast science as “the study of processes in atoms, molecules, or materials that occur in millionths of a billionth of a second or faster.” By the 1980s, the field had reached what seemed to be the upper limits of intensity. However, in 1985, Gérard Mourou, a French physicist and professor at the University of Rochester, was experimenting with even higher intensity laser pulses, looking for ways to increase intensity without rebuilding the laser. Mourou’s team was part of Rochester’s Laboratory for Laser Energetics (LLE), which was funded by the U.S. Department of Energy.
The eureka moment came, Mourou said, when he was riding a ski lift. As he saw the chairs on the lift spread and bunch, he realized he could do the same with the laser pulses. He hypothesized that spacing out and boosting the pulses before bringing them back together would result in higher-intensity laser pulses. Donna Strickland, one of only a handful of women pursuing a Ph.D. in physics at Rochester at the time, joined the Laboratory for Laser Energetics (LLE) and Strickland was assigned to Mourou’s ultrafast science group to help test his theory.
Donna Strickland (University of Waterloo)
Together, they developed chirped pulse amplification, or CPA, an optical technique that produces short, intense laser pulses that can vaporize precise points without causing collateral damage to the surrounding material. This discovery earned Mourou and Strickland half of the 2018 Nobel Prize in Physics. This development led to a dramatic escalation of peak intensities in laser technology, launching several new areas of research and practical applications.
In the Blink of an Eye
Mourou brought the CPA technique to the University of Michigan when he founded the Center for Ultrafast Optical Science (CUOS), a National Science Foundation Science and Technology Center from 1991 to 2001. At the time, they were using the technology to understand chemical reactions and to freeze those reactions – medical applications were far down the list of possibilities.
Detao Du
At CUOS, Dr. Mourou had several graduate students working in his lab including Detao Du, who joined the lab in 1993. Du recalls being assigned projects in the lab but also having the freedom to explore findings that caught his interest. During his quest to answer complex research questions, there was an incident that he tried not to dwell on. Du says he “must have been tired” one evening and accidentally lifted his goggles while aligning the mirrors of a femtosecond laser in the lab. This infrared laser emits burst of laser energy at an extremely fast rate. And thus, inadvertently making him vulnerable to some of the most powerful controlled bursts of energy produced in a laboratory at the time. Du says he caught a stray beam (not the main laser beam) and saw a flash. His instincts told him that although he experienced no visible damage to his eye, he needed to be checked out by a doctor to make sure there was no underlying damage.
Ron Kurtz
Du was examined at to the University of Michigan’s Kellogg Eye Center. That is where Ron Kurtz, a second-year medical resident, was called in to assess the injury. During the evaluation, Kurtz observed that the laser left a series of pinpoint laser burns in the center of his retina, very precise and perfectly circular, unlike other lasers in clinical use at that time. After observing the injury, Kurtz met with Mourou’s team, primarily to promote laser safety in the lab, but also to learn whether the lasers they were developing could be clinically useful. This collaboration would shed light on important observations regarding the damage thresholds for tissue and other materials using femtosecond laser pulses.
A Serendipitous Encounter
After a little over a year of conducting experiments, Ron Kurtz and Detao Du presented their findings at an optics conference in 1994. There they met Tibor Juhasz, a research scientist at the University of California, Irvine who happened to be investigating femtosecond laser applications in ophthalmology. Juhasz had also been a postdoctoral researcher in Mourou’s lab at the University of Rochester several years earlier in 1987. Soon after the conference he received an early morning phone call from his former mentor, inviting him to come to the University of Michigan to help develop femtosecond lasers for use in the eye.
By that time, the University of Michigan had also come to understand the potential of the work to have both societal impact and economic value and committed university research funds to help expand and accelerate the work. Additional funding came from NIH and NSF through the Small Business Innovation Research (SBIR) program. Together, Kurtz, Juhasz, and the CUOS lab contributed to developing of a novel approach to corrective eye surgery that left the surrounding tissue untouched.
Tibor Juhasz
By 1997, Kurtz and Juhasz founded IntraLase, a spinoff company that focused on commercializing the bladeless LASIK technique for refractive surgical procedures (also known as corrective eye surgery). Though there were several potential applications their startup could explore, they decided to focus on the cornea of the eye which seemed the most promising. The procedure they developed, uses a femtosecond laser instead of the manual blade that had previously been used to cut into the cornea before reshaping it to improve the patient’s focus.
By 2001, they launched the world’s first commercially available femtosecond laser after several years of successful clinical studies and eventual FDA clearance. The startup received initial seed funding from the Enterprise Development Fund of Ann Arbor and additional support from Small Business Innovation Research (SBIR) funding provided by both NIH and NSF as well as the university and its technology transfer office. In 2004, IntraLase went public and earned $84 million before it was acquired in 2007 for $808 million by Advanced Medical Optics. Later, IntraLase became the property of Johnson & Johnson Vision. To this day, IntraLase is considered one of the most successful startups incubated at the University of Michigan, according to Crain’s Detroit Business.
Setting the Standard and Emerging Applications
The femtosecond laser approach eventually replaced the mechanical blade and is now even catching up to the excimer laser, which has long been the standard laser for reshaping the eye. Due to the precision of the cut from the femtosecond laser, these bladeless approaches typically present fewer risks for complications compared to previous generations of procedures. Since its introduction, the number of procedures has grown to 2 to 3 million each year, with more than 30 million people having benefited from the technology to date. The development and widespread acceptance of a femtosecond laser for use in eye surgeries has led to laser vision correction being one of the most regularly performed surgeries in the country (and the world).
As a result of the lab incident and research done in the CUOS lab, many of those researchers, including Ron Kurtz and Tibor Juhasz, have continued to explore other potential applications of the femtosecond laser, particularly for common ophthalmic conditions and diseases including glaucoma and cataracts. In 2008, the two teamed up again to develop femtosecond laser cataract surgery; today, this technology is used in about 15 percent of cataract surgeries. Currently, a California start-up led by Juhasz, ViaLase, is developing new methods to treat glaucoma more effectively by using femtosecond lasers.
Thanks to their work, many of us are seeing a little bit more clearly these days.
By Meredith Asbury